Choosing medical temperature sensors requires exceptional caution, as accuracy, reliability, safety, and compliance directly impact patient health, diagnostic outcomes, and treatment efficacy. The following are critical points to focus on:
I. Core Performance Metrics
1. Accuracy & Precision:
- This is the most critical metric. Medical temperature measurements often demand very high precision (e.g., ±0.1°C or even ±0.05°C). Excessive error can lead to misdiagnosis or delayed treatment.
- Pay attention to the sensor's accuracy within the target operating temperature range (e.g., oral: 35-42°C, ambient: 15-30°C).
- Understand its long-term stability (drift) and repeatability.
2. Resolution:
- The smallest temperature change the sensor can detect/display (e.g., 0.01°C or 0.1°C). Higher resolution aids in monitoring subtle changes, especially in critical care or precise experiments.
3. Response Time:
- The time required for the sensor to reach the true temperature of the measured object (often expressed as a time constant, e.g., seconds to tens of seconds).
- Application Determines Need: Ear thermometers require very fast response (seconds), while core temperature monitoring or incubator measurements can tolerate slower response (tens of seconds to minutes).
4. Measurement Range:
- Ensure the sensor's operating temperature range fully covers the needs of the intended application (e.g., thermometers: 35-42°C, cryogenic storage: -80°C, high-temperature sterilization: >121°C).
II. Safety & Biocompatibility
5. Biocompatibility (For Contact Sensors):
- If the sensor directly contacts patient skin, mucous membranes, or bodily fluids (e.g., oral, rectal, esophageal, vascular catheter probes), it must comply with relevant medical device biocompatibility standards (e.g., ISO 10993 series).
- Materials should be non-toxic, non-sensitizing, non-cytotoxic, and withstand the intended disinfection/sterilization processes.
6. Electrical Safety:
- Must comply with stringent medical electrical safety standards (e.g., IEC 60601-1 and its collateral standards).
- Key considerations include insulation, leakage currents (especially patient-applied parts), defibrillation protection (if used in environments where defibrillation might occur), etc.
- Preventing electrical shock risks is paramount.
7. Disinfection/Sterilization Compatibility:
- What disinfection or sterilization methods must the sensor or its probe withstand (e.g., alcohol wipe, autoclaving, ethylene oxide (EtO) sterilization, low-temperature plasma sterilization)?
- Sensor performance and material integrity must remain stable after repeated disinfection/sterilization cycles.
8. Invasiveness Risk (For Contact Sensors):
- Consider risks associated with the method of use (e.g., mucosal damage, infection risk) and select probes with safe, well-designed configurations.
III. Environmental Adaptability & Robustness
9. Environmental Tolerance:
- EMI Resistance: In environments saturated with medical electronic equipment, the sensor must resist interference to ensure stable, accurate readings.
- Temperature/Humidity Range: The sensor itself needs to operate reliably within expected environmental conditions.
- Chemical Resistance: Can it withstand exposure to disinfectants, cleaning agents, bodily fluids, etc.?
10. Mechanical Robustness:
- Is it sufficiently rugged to endure routine use, cleaning, and potential drops or impacts (especially for handheld devices)?
- Are cables (if present) durable and connectors reliable?
IV. Regulatory Compliance & Certification
11. Medical Device Regulatory Certification:
- This is a mandatory requirement! Sensors, as medical devices or critical components thereof, must obtain regulatory approval for the target market.
- Major certifications include: US FDA 510(k) or PMA, EU CE Marking (under MDR), China NMPA registration, etc.
- Ensure suppliers provide valid certification documentation.
12. Relevant Standards Compliance:
- Compliance with pertinent international and national standards, such as IEC/EN 60601 series (electrical safety, EMC), ISO 13485 (Quality Management System), ISO 80601-2-56 (Particular requirements for basic safety and essential performance of clinical thermometers), etc.
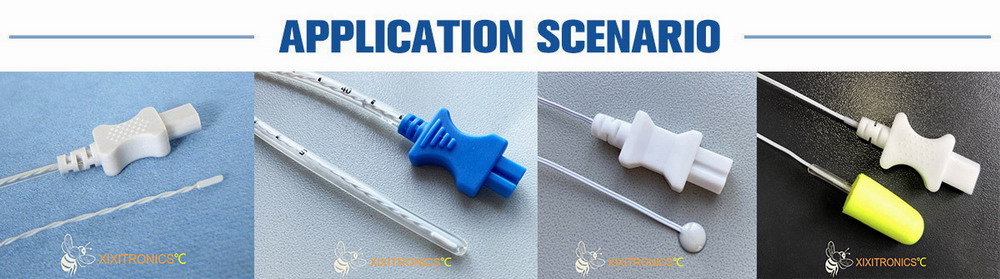
V. Application Scenario & Usability
13. Specific Application Requirements:
- Measurement Site: Body surface (forehead, axilla), body cavity (oral, rectal, ear canal), core (esophageal, bladder, pulmonary artery), fluids (blood, culture media), environment (incubator, refrigerator, sterilizer)?
- Measurement Mode: Continuous monitoring or spot-check? Contact or non-contact (infrared)?
- Integration Needs: Standalone device (e.g., thermometer) or integration into other medical equipment (e.g., patient monitor, anesthesia machine, ventilator, infant incubator, dialysis machine)? What interface type is needed (analog/digital)?
- Patient Population: Adults, children, neonates, critically ill patients?
14. Size & Shape:
- Is the probe size appropriate for the measurement site (e.g., neonatal rectal probes must be very thin)?
- Is the overall sensor size suitable for integration or handheld use?
15. Usability & Ergonomics:
- Is operation simple and intuitive? Is the display clear and easy to read?
- Is it comfortable and convenient for both patients and healthcare staff?
16. Maintenance & Calibration:
- What is the calibration interval? How complex is the calibration process? Does it require return to factory? Are self-diagnostic features available?
- What are the maintenance costs? Are consumables/spare parts (e.g., probe covers) readily available and cost-effective?
17. Cost:
- Consider initial procurement cost, maintenance costs (calibration, replacement parts), and total cost of ownership, while meeting all performance, safety, and regulatory requirements.
Summary & Recommendations
1.Define Requirements Clearly: First, precisely define your specific application scenario (what to measure, where, how, accuracy requirements, environmental conditions, target market regulations, etc.).
2.Prioritize Safety & Compliance: Biocompatibility, electrical safety, and medical device regulatory certification are non-negotiable red lines.
3.Accuracy & Reliability are Paramount: Verify precision, stability, and response time under target range and application conditions.
4.Consider the Full Lifecycle: Evaluate usability, maintenance costs (especially calibration), disinfection/sterilization requirements, and durability.
5.Choose a Reliable Supplier: Select suppliers with proven experience in the medical field, good reputation, and the ability to provide comprehensive technical support and compliance documentation. Understand their Quality Management System (e.g., ISO 13485 certified).
6.Prototype Testing: Conduct thorough testing and validation in the actual application environment or simulated conditions before finalizing the selection.
Medical applications leave no room for error. Selecting a temperature sensor requires carefully weighing all key points to ensure it is safe, accurate, reliable, and compliant, thereby truly serving medical diagnosis and patient health. If you have a specific application scenario, I can provide more targeted advice.
Post time: Jul-29-2025